Over the past 1.5 billion years, complex life forms, including plants, fungi, and animals, have evolved from a shared ancestral lineage. These organisms, known as eukaryotes, possess cells with nuclei and other structures that support the development of intricate biochemical systems. Because of this common origin, there is a striking overlap in the molecular architecture of life: many of the compounds synthesized by animals echo the forms and functions of molecules found in plants and fungi. This biochemical kinship helps explain why certain herbs and mushrooms can exert such profound effects on human physiology, cognition, and mood.
Take, for instance, the porphyrin ring structure, a fundamental biochemical scaffold shared by plants and animals alike. In plants, porphyrin binds magnesium to form chlorophyll, capturing solar energy through photosynthesis. In animals, porphyrin binds with iron to form heme, the oxygen-carrying core of hemoglobin and a key component in mitochondrial respiration. Despite serving different functions, both systems rely on the same molecular architecture to manage life’s energetic demands.
Another example of this shared biology is exemplified by auxin, a plant hormone that governs growth and development in response to sunlight. It is structurally similar to serotonin, the mammalian neurotransmitter that modulates mood, circadian rhythm, and sensory processing. These parallels reveal an evolutionary language spoken across species, where the biochemistry of perception, growth, and transformation shares deep common roots. Seen this way, the psychotropic effects of certain botanical and fungal compounds appear not as accidental anomalies, but as resonant expressions of a deep, molecular kinship.
Over millions of years of co-evolution, plants and fungi developed an extensive repertoire of defensive compounds known as allelochemicals, which serve to deter predators, suppress competitors, and resist pathogens. Among the most potent of these are the bitter-tasting alkaloids: nitrogen-containing molecules that, while often toxic in higher doses, interact strongly with mammalian physiology—particularly the brain and digestive tract. In turn, mammals, including early hominids, evolved a range of physiological defences to limit toxicity, such as the bitter taste receptor, the vomiting reflex, and hepatic detoxification. Through careful observation and experimentation, our ancestors augmented these physiological defences to further reduce risk of toxic exposure. This included selecting less harmful species, combining ingredients synergistically, and using various methods of preparation including grinding, soaking, fermentation, leaching and cooking to neutralize their harmful effects.
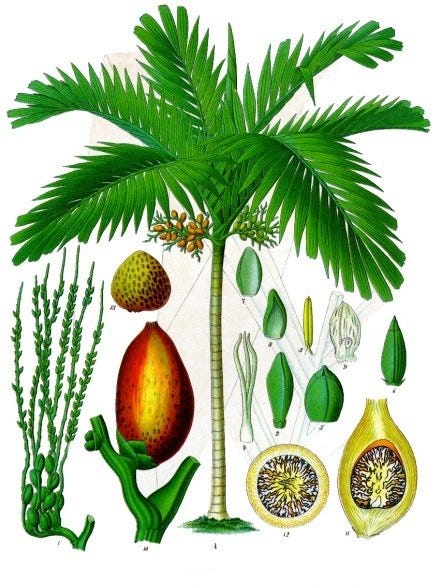
These behavioural innovations transformed allelochemical deterrents into allies, laying the groundwork for medicinal and ritual use. Across nearly every region of the world, human cultures have adopted psychotropic plants and fungi, not merely to survive, but to awaken, heal, and understand the world around them. Betel nut (Areca catechu), rich in arecoline, has been used for over 10,000 years as a narcotic and digestive stimulant in Southeast Asia. Coca (Erythroxylum coca), domesticated in the Andes, contains small amounts of the alkaloid cocaine, and is used to enhance endurance and mood in high-altitude environments. In North America, the nicotine-containing tobacco (Nicotiana tabacum) was used extensively by Indigenous peoples for ceremonial and spiritual purposes, with archaeological evidence dating back over 12,000 years. From khat (Catha edulis) in East Africa to iboga (Tabernanthe iboga) in the Congo Basin, from peyote (Lophophora williamsii) in Central Mexico to ayahuasca in the Amazon, humans have long cultivated important relationships with alkaloid-rich plants and fungi.



This deep integration of these psychotropic plants and fungi into human society is not merely cultural, but neurobiological. The presence of endogenous receptors for compounds like nicotine, muscarine, serotonin, dopamine, cannabinoids, and opioids points to more than just biochemical compatibility; it suggests a long evolutionary dialogue between human physiology and the psychotropic chemistry of plants and fungi. Some evolutionary theorists propose that these substances may have supported the energetically demanding processes of neurochemical signaling in the human brain, enhancing cognitive function, emotional regulation, and social cohesion. Others highlight their influence on the emergence of shamanic practices, mythopoetic imagination, and the symbolic systems that undergird early human civilization.
These compounds did more than alter individual minds, they shaped how we relate to suffering, transformation, and the enigma of death. The ritual use of psychotropics, from initiatory rites to ancient funerary practices, reflects a deep-rooted human impulse to seek meaning through altered states of consciousness. Such substances became not just agents of survival, but tools for crossing existential thresholds—illness, grief, rebirth, and mortality itself. Among them, few have captured the modern imagination as vividly as psilocybin, the tryptamine alkaloid found in so-called “magic mushrooms,” structurally akin to serotonin and capable of evoking experiences that seem to touch the very foundation of what it means to be human.
The Chemistry of Psilocybin
Among the fungi, Psilocybe mushrooms stand out for their unique biosynthetic capacity to produce psilocybin—a tryptamine alkaloid that is structurally similar to serotonin (5-hydroxytryptamine or 5-HT). Once ingested, psilocybin is rapidly converted into psilocin, its active form, which binds primarily to 5-HT₂A receptors in the brain. These receptors are not just implicated in the psychedelic experience, but play a key role in mood, perception, imagination, memory, and cognition.
This receptor affinity helps explain the broad-spectrum effects of psilocybin: from enhanced sensory awareness and synesthesia to ego dissolution, emotional catharsis, and visionary states. Unlike classic stimulants or sedatives, psilocybin’s action is neither unidirectional nor predictable, often revealing what is hidden from our conscious minds.
This same receptor profile also confers a powerful anti-inflammatory and neuroprotective effect. The 5-HT₂A receptor is present not only in the central nervous system but also in immune cells, blood vessels, and the gastrointestinal tract, pointing to psilocybin’s systemic impact. This is partly why many patients with chronic illness—including cancer, IBS, and fibromyalgia—report not just improvements in mood after or while taking psilocybin mushrooms, but changes in pain perception, digestion, and immune function.
A Renaissance of Research
After several decades of prohibition, clinical research into psilocybin has surged over the past 15 years. Several high-quality studies have now shown what traditional medicine has long understood: that psilocybin mushrooms have significant therapeutic value, especially in the treatment of mood disorders.
One landmark study conducted a randomized controlled trial using two psilocybin-assisted therapy sessions (20 mg/70 kg and 30 mg/70 kg) for individuals with major depressive disorder. Depression scores dropped rapidly and significantly, with lasting effects persisting at the four-week follow-up (Davis et al. 2021).
In a six-week randomized, double-blind trial comparing psilocybin with the SSRI escitalopram, both groups showed improvement, but the psilocybin group experienced greater secondary outcomes such as emotional resilience, meaning, and connectedness (Carhart-Harris et al. 2021).
In terminal illness, psilocybin has shown exceptional promise. A placebo-controlled crossover study demonstrated that a single 0.3 mg/kg dose significantly reduced anxiety, and depression in patients with cancer, with 60–80% maintaining improved mental health outcomes after six months (Ross et al. 2016).
Even at very low doses, psilocybin demonstrates measurable pharmacological activity. PET imaging studies have shown that just 3 mg of psilocybin produces approximately 43% occupancy of the 5-HT₂A receptor, enough to induce mild perceptual changes (Madsen et al. 2019). This challenges the widespread belief that “microdoses” are ineffectual. Given that Psilocybe cubensis typically contains 0.6–1.2% psilocybin by dry weight, a frequent recommendation of 250 mg exceeds the threshold for a true microdose. Instead, the research suggests that an effective microdosing range lies between 40 and 160 mg of dried mushroom—or the equivalent in a standardized extract—depending on the strain and individual sensitivity.
Beyond Mood: Addiction, Cognition, and Neuroplasticity
The therapeutic potential of magic mushrooms extends well beyond treating depression. A growing body of research highlights their efficacy in addressing addiction, obsessive-compulsive behavior, migraine, and even age-related cognitive decline.
In an open-label pilot study, psilocybin significantly reduced alcohol use among participants with alcohol use disorder. Two doses administered over 12 weeks with motivational enhancement therapy was shown to lead to a 26% decrease in heavy drinking days (Bogenschutz et al. 2015). A preclinical study revealed the underlying mechanism: psilocybin restores expression of metabotropic glutamate receptors (mGluR2) in the prefrontal cortex, reversing alcohol-seeking behavior and improving cognitive flexibility (Meinhardt et al. 2021).
Case reports have also demonstrated efficacy in obsessive-compulsive disorder (OCD). One particularly illustrative example documented a man with treatment-resistant OCD who found long-lasting symptom relief from biweekly psilocybin use (Wilcox 2014).
Migraine and cluster headache sufferers have likewise reported benefit. A small placebo-controlled crossover trial found significant reductions in migraine days following low-dose psilocybin (0.143 mg/kg), without adverse effects (Schindler et al. 2021).
Yet perhaps the most exciting frontier is psilocybin’s role in enhancing cognition and promoting neuroplasticity. Several neuroimaging and behavioral studies have demonstrated measurable improvements in cognitive fluency, originality, and brain network integration following both microdoses and macrodoses. In one fMRI study, a single psilocybin session increased connectivity between the ventromedial prefrontal cortex and the default mode network, with these changes persisting more than five weeks after dosing (Carhart-Harris et al. 2017).
On a cellular level, animal research has shown that psilocybin increases dendritic spine growth in the medial frontal cortex, with a single dose resulting in ~10% greater spine density, sustained for at least a month (Shao et al. 2021). These findings suggest psilocybin doesn’t just modulate perception, it literally changes the architecture of the brain.
Hipsilo: A Herbalist’s Approach to Microdosing
While interest in psilocybin continues to surge, its practical use, especially with respect to microdosing, remains uneven. Many commercial products rely on encapsulated mushroom powder, which is often poorly standardized, overdosed, and difficult to digest due to chitin, a fibrous polysaccharide that can irritate the gut. In an essay I wrote back in 2015, Love, Death, and Magic Mushrooms, I shared a deeply personal account of how psilocybin mushrooms impacted my own family and how I began to develop a microdosing protocol at a time when there was no published research or clinical precedent. What emerged was an innovative, life-saving intervention born of necessity, well before psilocybin was in the spotlight.
What came out of those early experiments was an extract that I later called Hipsilo, which stands for Herbal-Infused Psilocybin. It is an aqueous-citric acid extract formulated for microdosing, integrating psilocybin mushrooms with carefully selected herbs to support specific neurochemical and constitutional profiles. These formulas reflect over a decade of clinical use, drawing on principles from traditional herbal medicine:
Hipsilo(A) combines an aqueous-citric acid extract of Psilocybe cubensis with Syrian rue (Peganum harmala) tincture, a natural MAO-A inhibitor traditionally used across West Asia for its antidepressant and visionary properties. This blend is best suited for more severe unipolar depression marked by inertia, lack of motivation, and difficulty initiating action.
Hipsilo(B) was designed for patients with depression coupled with anxiety. It combines an aqueous-citric acid extract of Psilocybe cubensis with a high-CBD, low-THC Cannabis sativa extract to calm the nervous system and soften overactivity in the limbic circuitry. While I had very good results with this, due to regulatory barriers, sourcing issues, and increased costs, I haven’t been able to keep this formula in stock on a regular basis.
Hipsilo(C) is formulated with “medhya” (cognitive-enhancing) herbs from the Āyurvedic tradition, including brahmi (Bacopa monnieri), ashwagandha (Withania somnifera), and vacha (Acorus calamus), along with reishi mushroom (Ganoderma lucidum), one of my favourite Chinese medicinal herbs for anxiety and cognitive issues. One difference between it and Hipsilo(A) is that it excludes natural MAOIs like Syrian rue, making it generally safer when considering potential interactions, and is specifically helpful in anxiety and for cognitive decline.
Each extract is standardized by weight and concentration. For both versions, a 2.5 mL (½ tsp) dose provides approximately 125 mg of Psilocybe cubensis, and about 400 mg of the other medicinal herbs, placing it in an optimal range for microdosing. For more sensitive individuals, I typically recommend starting with 1.25 mL (¼ tsp), then using the dropper to titrate upward until the desired effect is achieved. The fluid extract format ensures consistent absorption and precise titration, supporting a flexible, individualized approach that can evolve with the patient’s needs.


Given that I have now over a decade of clinical use with these extracts, I have developed a significant body of empirical evidence to back up their use. And somewhat surprisingly, the extraction method I have evolved has proved to be remarkably shelf-stable. Anyone familiar with magic mushrooms knows well their limited shelf life, which in their whole, unprocessed form, typically lose potency within 6-12 months after harvest. In contrast, I have had patients contact me five years after obtaining the Hipsilo extract, only to report that it “works” just as it did when they first received it.
Clinical Use: From Protocol to Practice
In clinical practice, psilocybin mushroom’s greatest value may lie in its flexibility. While macro-dosing has garnered attention, and has played an important role in my own practice, the consistent, calibrated use of microdoses—especially when combined with supportive therapy, nutrition, and botanical medicine—holds significant promise for long-term transformation.
In my practice, I’ve employed both macro- and micro-dosed extracts for over a decade, in cases involving depression, trauma, anxiety, traumatic brain injury (TBI), and post-SSRI withdrawal. This makes Hipsilo particularly useful in complex cases where conventional medications have failed or introduced new complications.
Take the case of a 59-year-old woman presenting with fatigue, musculoskeletal pain, obesity, and chronic oversleeping. Though suspiciously diagnosed with “liver flukes,” her clinical picture instead suggested systemic sluggishness and hypometabolic depression. With lifestyle interventions (early rising, cold plunges, low-carb nutrition), my Liver formula, and twice-daily Hipsilo(A), she reported significant improvements in energy, appetite regulation, and mood within two weeks. By six weeks, her desire to nap had disappeared entirely—something she hadn’t experienced in years. Like most patients, her significant and lasting improvement meant that it wasn’t necessary to continue taking Hipsilo ad infinitum.
In another case, a 33-year-old First Nations male with TBI, chronic depression, and daily cannabis use had failed multiple attempts to taper off sertraline. With dietary support, craniosacral therapy, and Hipsilo(A), he successfully discontinued the SSRI within 24 hours without withdrawal symptoms. Though some cognitive challenges persisted, he later reported a profound healing experience during a higher-dose journey, reconnecting with ancestral memory and aligning more deeply with personal health goals.
A third patient, a 17-year-old woman navigating OCD, depression, and family trauma, was struggling under the burden of antidepressants and household responsibilities. After shifting to a whole-food diet, implementing creative expression and Reiki as somatic anchors, she was able to use Hipsilo(C) to wean herself off of citalopram. Her correspondence with me became increasingly optimistic, and within months, she reported positive shifts in focus, diet, and hope for her future.
These cases illustrate what I explored in my 2015 essay, Love, Death, and Magic Mushrooms: that the true potential of psilocybin lies not in its chemical novelty but in its ability to help people re-inhabit their lives: more connected to their bodies, relationships, and sense of meaning.
Safety, Dosage, and Contraindications
Despite its promise, any psilocybin-containing product must be approached with respect and caution. The principal safety concern lies in interactions with serotonergic drugs, especially SSRIs, SNRIs, MAOIs, tricyclics, triptans, and certain opioids. Combining these medications with psilocybin may precipitate serotonin syndrome—a rare but potentially life-threatening condition marked by agitation, tremor, hypertension, and confusion. However, there is the potential for any adverse effect to occur with any medication, so caution and careful consideration is always warranted.
Other contraindications include:
psychosis or a personal/family history of schizophrenia
insomnia (avoid late-day dosing)
mold or penicillin allergies (due to fungal origin)
unmanaged anxiety (microdosing may exacerbate restlessness early on)
For cultivated Psilocybe cubensis, a macrodose typically ranges from 3–10 grams of the dried fruiting body, usually taken on an empty stomach for ego dissolution or psychological reset. In contrast, microdose generally ranges from 50–150 mg of dried material (average 125 mg), best administered in the early morning on an empty stomach, and optionally no later than 4:00 p.m.
As an additional note of caution, it’s important to remember that even at low doses, psilocybin mushrooms may unearth unresolved trauma and could possibly destabilize fragile psychological states. Thus, while psychedelics such as magic mushrooms are part of our human birthright, it is best to seek out qualified and experienced clinical supervision for any macro- and micro-dosing protocol.
Towards a New Psychobotany
I don’t claim that psilocybin mushrooms are a miracle cure, but they are a remarkable therapeutic tool, especially when integrated into a broader framework that includes nutrition, botanical medicine, counseling, and movement. What sets my clinical approach apart is precisely this integration. Formulas like Hipsilo(A) and Hipsilo(C) aren’t defined solely by their psilocybin content, but by their synergy and the dynamic interplay between mushroom and herb, where traditional wisdom and modern science, inner transformation and outer support, come together in therapeutic alignment.
We stand at the threshold of a new psychobotany, where ancient plant traditions intersect with the insights of modern neuroscience. While the commercial potential of psilocybin is drawing significant attention, the deeper opportunity lies elsewhere: not in reducing it to just another pharmaceutical, but in restoring it to a living tradition of healing. One that is relational, respectful, and rooted in the whole person. This is the essence of traditional herbal medicine: not the mere isolation of compounds, but in the cultivation of relationships with the plants and fungi that have accompanied us on our long, evolutionary journey.
Interested in deepening your studies?
If you’re a practitioner or a student, earn a certificate in the therapeutic use of magic (psilocybin) mushrooms through the Dogwood School of Botanical Medicine.
References
Bogenschutz MP, Forcehimes AA, Pommy JA, et al. Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study. J Psychopharmacol. 2015;29(3):289–299.
Carhart-Harris R, Giribaldi B, Watts R, et al. Trial of Psilocybin versus Escitalopram for Depression. N Engl J Med. 2021;384(15):1402–1411.
Carhart-Harris RL, Roseman L, Bolstridge M, et al. Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms. Sci Rep. 2017;7(1):13187.
Davis AK, Barrett FS, May DG, et al. Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78(5):481–489.
Madsen MK, Fisher PM, Burmester D, et al. Psychedelic effects of psilocybin correlate with serotonin 2A receptor occupancy and plasma psilocin levels. Neuropsychopharmacology. 2019;44(7):1328–1334.
McKenna T. Food of the Gods: The Search for the Original Tree of Knowledge. New York: Bantam; 1992.
Meinhardt MW, Pfarr S, Fouquet G, et al. Psilocybin targets a common molecular mechanism for cognitive impairment and increased craving in alcoholism. Sci Adv. 2021;7(47):eabh2399.
Prochazkova L, Lippelt DP, Colzato LS, et al. Exploring the effect of microdosing psychedelics on creativity in an open-label natural setting. Psychopharmacology (Berl). 2018;235(12):3401–3413.
Ross S, Bossis A, Guss J, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30(12):1165–1180.
Schindler EAD, Sewell RA, Gottschalk CH, et al. Exploratory Controlled Study of the Migraine-Suppressing Effects of Psilocybin. Neurotherapeutics. 2021;18(1):534–543.
Shao LX, Liao C, Gregg I, et al. Psilocybin induces rapid and persistent growth of dendritic spines in frontal cortex in vivo. Neuron. 2021;109(16):2535–2544.e4.
Wilcox JA. Psilocybin and Obsessive Compulsive Disorder. J Psychoactive Drugs. 2014;46(5):393–395.
Winkelman MJ. Introduction: Evidence for entheogen use in prehistory and world religions. J Psychedelic Stud. 2019;3(1):1–20.







