It’s been a dark couple weeks—not only due to recent political events—but here on the “Sunshine” Coast of BC, it’s been an onslaught of storming weather interspersed with misty grey days, with not more than a few of hours of sun to cast out the dark. Of course, it’s to be expected here in the Pacific Northwest, and I count my blessings compared to friends in southern climes who face more existential issues like access to fresh water. So I know it sounds ungrateful, but holy crap—I am done with all this rain!
It doesn’t help that I kinda live in a marsh, with a rich clay-loamy soil that is great for growing but becomes a wetland with just a few days of continuous rain. Last January my basement flooded from a crazy rain-hail storm that choked up my perimeter drain, so this year, I did some serious drainage work. This included directing my downspouts away from the house, and building a 300’ open French drain with 15 tons of gravel to channel water out of my yard. I spent months watching French drain videos on YouTube and learned a lot, watching just enough to get slightly emotionally invested in two competing French drain gurus—one from Florida and the other from Michigan—who would talk shit about each other in their videos. But I took their critiques to heart, and hopefully, I synthesized the best from each. I think there may be a lesson in that.
But the darkness that motivates me to write today is only symbolized by this dismal weather. While the current political reality isn’t what I was hoping for, I wasn’t surprised by the turn of events. The neurological and sociological inflammation of the global pandemic has created a problem not just for political incumbents, but fomented a rightward tilt towards intolerance and hate. From the Hindutva in India and the rise of the AfD in Germany, to the alt-right movement in the US that trolls women with phrases like “your body, my choice”—all while legislating impediments to full and timely access to women’s health care—it’s a worrisome trend. This embrace of fascistic ideologies and authoritarianism begs the question of what exactly our grandparents were fighting for during the Second World War.
Masculinity in crisis?
In many respects this has nothing to do with politics; rather, it is a manifestation of masculinity in crisis. Or maybe that’s going too far—perhaps it’s just the same old cycle, swinging back to the worst of its tendencies. I prefer to think of it as masculinity in crisis if only because it provides a little hope, that we can eventually shift back towards a state of balanced masculine power. Although it’s hard to believe with the globe’s apparent embrace of authoritarianism, I believe most people yearn for leaders grounded in the ethics of peace, prosperity, and social justice: a leader that expresses love and respect for each person, regardless of their differences. In a man, this is manifest in his ability to protect those weaker than himself, embodying the archetype of a loving, wise and just leader.
In the ancient Chinese text the Tao Te Ching, the feminine principle of yin is described as more powerful than that of yang, even if hiding itself as an amorphous mystery that is only understood through the contemplation of mind. According to this realization, the ideal leader is someone who expresses this yin quality: coming reluctantly to power, being of service not for personal gain but as a response to a vital need; to restore balance and integrity. Such humility is almost impossible to find in today’s political and business leaders—indeed, the character and ethos of the broligarchy couldn’t be more different. Their immature leadership has spawned a generation of young men who think misogyny and trolling are somehow “cool,” slipping into a cesspool of toxic masculinity. It’s little surprise that the South Korean 4B movement has become a global trending topic—no dating, no sex, no marriage, and no babies—women are putting their foot down.
The ideal of masculinity expounded by the ancient Chinese philosophers is perhaps an impossible standard, but there are recent examples that come close. One is José "Pepe” Mujica, former president of Uruguay (2010-2015), formerly described as "the world’s humblest head of state" due to his simple lifestyle, and by donating 90% of his salary to impoverished communities. In this era of late-stage capitalism, Mujica has been an outspoken critic of concentrating wealth in the hands of a few, and reminding us that focusing on material possessions does not bring us happiness. Far from being a lofty idealist, Mujica is very much a pragmatist, fighting for and enacting policies that have brought about social and economic justice in Uruguay.
While Mujica’s core values align with Chinese philosophy, he certainly isn’t some kind of “soy boy”, and is known for his rancorous love of soccer, not above cussing out officials that make judgments against his favourite team. In this way, balanced masculinity doesn’t need to conform to a particular archetype or cultural behaviour, just that it remains true to actions that prevent and resolve suffering—especially in the most vulnerable. Other modern examples of positive male role models in leadership include Nelson Mandela (South Africa), John Lewis (United States), Olof Palme (Sweden), Lech Wałęsa (Poland), Sergio Vieira de Mello (Brazil), and Vaclav Havel (Czechoslovakia).
In the future, I want to spend more time exploring masculinity and this crisis among young men in particular, as they stumble in their search to feel aligned, on purpose, and self-actualized. But in deference to the feminine principle alluded to earlier, and to address the reality of the moment, I want to take some time to appreciate women, and one group in particular…
Perimenopausal Women
I have recently been lecturing on the subject of perimenopause. I usually begin my talk by saying that I wouldn’t have a career if not for perimenopausal women, who probably make up about 50% of my practice. I’ve spent some time thinking about why this is, and have come to the conclusion that as women pass through this phase, they undergo a kind of psychological death—commensurate with the cessation of ovulation—which gives them the opportunity to gaze upon the whole of experience. Inevitably, this perspective facilitates an awareness of the interconnectedness of things, and hence, many are drawn to a holistic way of thinking, including the use of natural products such as herbs to restore balance.
Given the almost 30 years I have been working with this cohort, I’ve learned a lot about how to understand and manage perimenopause. First off, I think it’s important to address the fact that it is not a pathology, as is often characterized in modern medicine—involving invasive interventions such as surgery and powerful hormonal drugs—but a natural transition that, in most cases, can be supported and balanced naturally.
Also known as the “climacteric,” menopause is the stage in a woman’s life when the menstrual cycle ceases, marking the end of her reproductive phase, arising from the depletion and aging of a finite number of oocytes (or “eggs-in-waiting”) in the ovaries. Perimenopause is the transitional phase before menopause, marked by hormonal fluctuations, and especially a decline in estrogen and progesterone levels. This stage typically begins in a woman’s 40s but can start as early as the late 30s or as late as the mid-50s, lasting 4-10 years. Menopause itself is confirmed when there is no menstrual bleeding for a year, indicating decreased hormone production by the ovaries, often confirmed by measuring hormone levels in blood or urine.
Over the years, I have observed that, on an individual basis, the severity and duration of perimenopausal symptoms can vary enormously. Differences can also be seen across different racial and ethnic groups, with African-American and Hispanic women reported to experience more severe symptoms, while Asian women often reporting fewer symptoms. While these racial and ethnic differences may relate to genetic factors, I think much relates to modifiable risk factors such as diet and lifestyle.
While menopause is a natural and inevitable stage of life, there are certain conditions that can accelerate menopause, including autoimmune and genetic conditions—about 1-2% of women—as well as surgical interventions such as hysterectomy, ablation, and embolization (used for fibroids and excessive menstrual bleeding).
One of the key indicators of the perimenopause stage are changes in bleeding patterns, driven by changes in hormone levels. In her reproductive years, a woman's ovaries produce estradiol, progesterone, and testosterone in a cyclical manner, regulated by follicle-stimulating hormone (FSH) and luteinizing hormone (LH) released from the pituitary gland. As menopause approaches, the depletion of oocytes creates a positive feedback loop, raising circulating FSH and LH levels due to fewer responsive oocytes. In this way, estradiol levels may remain stable or even slightly increased compared to fertile years, but as ovulation begins to fail, progesterone levels typically decrease, often resulting in a relative estrogen excess, with either shorter or irregular menstrual cycles. Once ovarian hormone production ceases entirely, estrogen production comes from fatty tissues via the aromatase enzyme, as well as in smaller amounts produced in the bone, blood vessels, and brain.
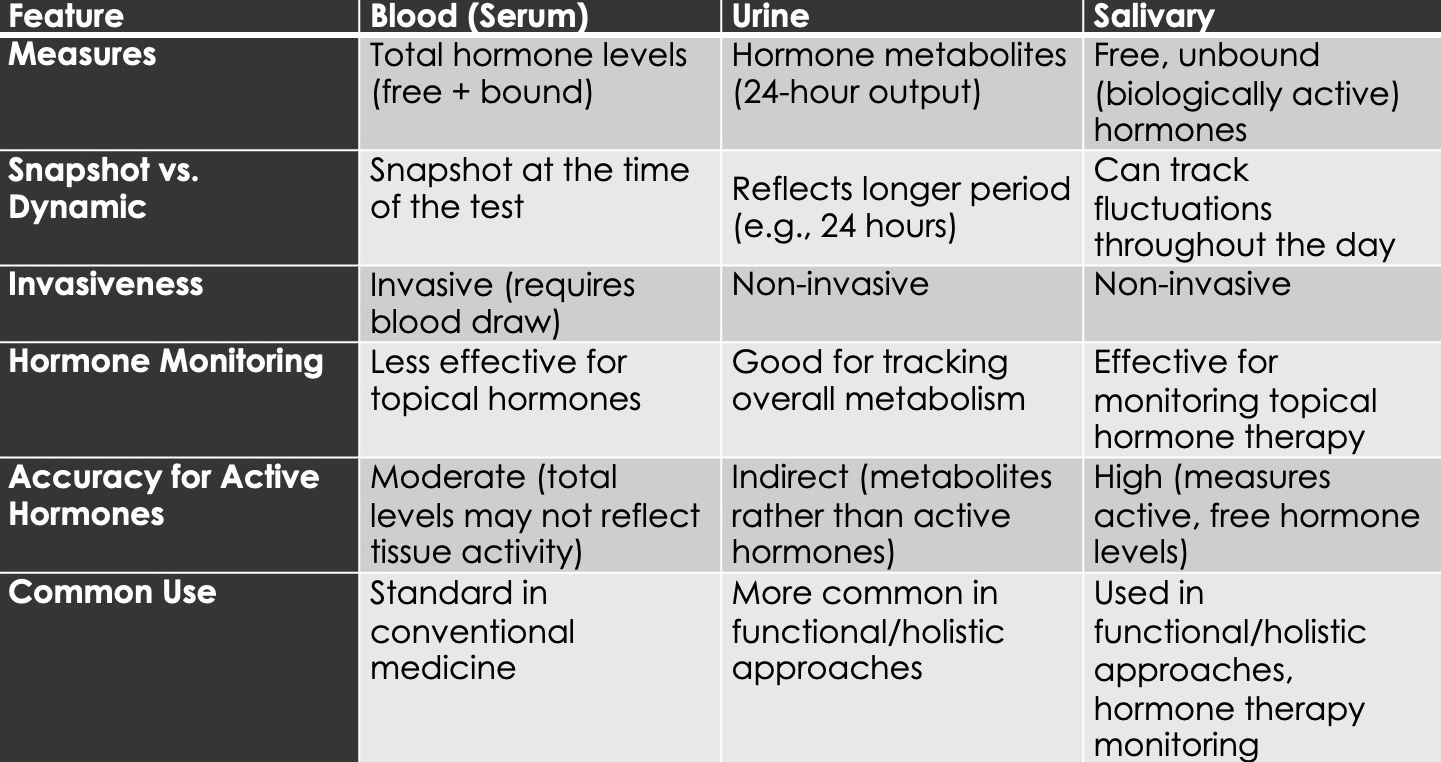
Given that estrogen and progesterone levels can fluctuate widely during perimenopause, it makes it difficult to capture a consistent picture with the kind of blood tests typically favoured by medical physicians. Research shows that blood hormone levels may not accurately reflect tissue levels, even if we take care to distinguish between bound and free hormone forms. At best, blood hormone levels provide only a snapshot and do not fully reflect tissue activity. Such tests are often used to measure the impact of hormone drugs, which have to be given in high doses due to the fact that as little as 20% actually makes it into the bloodstream. While necessary in some cases, oral hormone drugs are my least favoured intervention because they significantly add to the toxic burden of the liver.
Other testing methods I prefer include urine and salivary testing. Urine tests measure hormone metabolites, providing an inferential model of hormone output over a 24-hour period. In contrast, salivary tests measure free, unbound hormone levels, capable of capturing hormone fluctuations throughout the day. Salivary tests are particularly useful for tracking daily rhythms and monitoring topical hormone therapies like progesterone cream, that do not raise serum hormone levels significantly, but nonetheless exert their benefits at the tissue level. When hormone therapy needs to be considered, I prefer to recommend such topical preparations, which bypass the liver, and hence, require a much lower dose to be effective.
There are a large number of perimenopausal symptoms, including hot flashes, sleep disturbances, mood changes, vaginal dryness and atrophy, changes in libido, irregular periods, metabolic changes, osteoporosis, cardiovascular disease, cognitive changes, hair and skin changes, and urinary issues. The following is a review of each issue and some interventions that I commonly use, but by no means does it represent everything I can think of. And as mentioned above, I do recommend topical progesterone creams periodically, but only after the interventions below have failed to yield results.
Hot Flashes and Night Sweats
Hot flashes are sudden, intense sensations of heat, often accompanied by sweating, palpitations, and flushing, typically occurring at night and disturbing sleep. Declining estrogen levels affect the hypothalamus, making it more sensitive to slight changes in body temperature, which can trigger vasodilation and sweating. Lower estrogen levels are also associated with increased sympathetic nervous system activity (the “fight or flight” response), which further contributes to vasodilation.
I have theorized that hot flashes may be a biological response to activate thermogenic mechanisms, which encourages estrogen synthesis in fatty tissues by enhancing peripheral aromatization. A general observation is that women that have sufficient body fat experience fewer or less severe hot flashes, whereas women with a very low body fat percentage may experience worse symptoms, driven by the body trying, unsuccessfully, to synthesize more estrogen from depleted fat stores.
Holistic Interventions:
Diet: phytoestrogens (e.g., legumes, sprouts, flax seed)
Herbs: shatavari, peony, chasteberry, dang gui, American ginseng, black cohosh, red clover, sage, licorice
Nutrients: B complex, vitamin E, evening primrose oil, omega 3 fatty acids
Lifestyle: avoid triggers such as caffeine, alcohol, and spicy foods
Sleep Disturbances
Difficulty falling or staying asleep is common in perimenopause, often due to night sweats or anxiety. Hormonal fluctuations can affect neurotransmitters, including serotonin and GABA, disrupting sleep cycles, and night sweats may further exacerbate insomnia. One interesting phenomena is that sleep is affected by diurnal serotonin levels, and specifically, it’s a little surge of serotonin during REM stage sleep that drives us into the restorative, deep cycle sleep. Thus, ensuring healthy serotonin levels during the day — through exercise and sun exposure — can help promote restorative sleep.
Holistic Interventions:
Diet: elimination/challenge diet, healthy fats, probiotic foods; avoid refined carbohydrates
Herbs: chamomile, reishi, skullcap, hops, passionflower, valerian, California poppy, kava, CBD/cannabis (with caution)
Nutrients: magnesium, melatonin, 5-HTP, L-theanine, GABA
Lifestyle: mindfulness meditation, relaxation techniques, daily physical exercise
Mood Changes
During perimenopause many women experience emotional fluctuations, including increased irritability, sadness, or anxiety. Reduced estrogen and progesterone impact neurotransmitter activity, affecting serotonin, dopamine, and norepinephrine levels, which can lead to mood swings, anxiety, and depression. Apart from this, the life change and loss of fertility can trigger feelings of despair and sadness.
Holistic Interventions:
Diet: elimination/challenge diet, healthy fats, probiotic foods, avoid alcohol
Herbs: chai hu, bacopa, ashwagandha, reishi, St. John’s Wort (SJW), damiana, psilocybin (microdosing)
Flower Essences: cerato (for self-esteem), mimulus (for fear), gorse (for hopelessness), mustard (for melancholy), red chestnut (for worry), rock rose (for panic), sweet chestnut (for despair)
Nutrients: B complex, vitamin D3, magnesium, omega 3 fatty acids, 5-HTP
Lifestyle: regular exercise, exposure to sunlight (UVA/B), intimacy with friends or partners, counseling and therapy, abhyanga (self-massage), aromatherapy
Vaginal Dryness and Atrophy
Discomfort, itching, or burning in the vaginal area often arises during intercourse due to the thinning and drying of vaginal tissue. Lower estrogen levels lead to thinning of the vaginal lining, reduced lubrication, and a loss of elasticity, resulting in vaginal atrophy.
Holistic Interventions:
Diet: adequate protein, healthy fats, phytoestrogenic foods (e.g., legumes, sprouts, flax seed)
Herbs: shatavari, peony, dang gui, American ginseng, black cohosh, red clover, licorice
Nutrients: B complex, vitamin E, evening primrose oil (EPO), omega 3 fatty acids, ceramides, collagen
Lifestyle: yoni abhyanga (self-massage for the vaginal area) with nourishing oils, e.g. coconut, jojoba, shea, coco, almond; these oils can also be medicated with the appropriate herbs
Changes in Libido
Decreased sexual desire or interest is a common experience during the perimenopausal transition, as lower estrogen and testosterone levels can reduce sexual desire, arousal, and satisfaction. While it is normal and expected change for many woman, others may want to maintain an active sex life.
Holistic Interventions:
Diet: adequate protein, healthy fats
Herbs: shatavari, peony, chasteberry, shu di huang, dang gui, ashwagandha, American ginseng, milky oat, damiana, licorice, chocolate
Nutrients: B complex, vitamin D3, selenium, zinc
Lifestyle: sexual counseling, emotional intimacy, humor
Irregular Periods
During perimenopause, menstrual cycles become unpredictable in length, frequency, and flow as ovulation becomes more erratic. This irregular ovarian function leads to fluctuating hormone levels, which results in irregular periods.
Holistic Interventions:
Herbs: shatavari, peony, chasteberry, shu di huang, dang gui, licorice, bupleurum, dandelion root
Nutrients: B complex, magnesium
Lifestyle: abdominopelvic exercise (e.g. belly-dancing); obervance of daily rhythms
Metabolic Changes and Weight Gain
Hormonal changes and a slowing metabolism often lead to an increase in truncal-abdominal fat, making weight loss more difficult. Lower estrogen levels slow metabolism and promote fat accumulation, which is compounded by insulin resistance (metabolic syndrome) and elevated cortisol from chronic stress. An important trend to reverse with aging is sarcopenia, or a loss of muscle mass, which over the age of 50 occurs at a rate of between 1-3% each year. This gradual loss of muscle mass has an unfavourable influence on metabolism and promotes weight gain.
While it is normal for perimenopausal women to accumulate some fat, needed for estrogen synthesis, it’s important to maintain a waist to hip ratio of less than 80% to ensure good metabolic health — no matter your age.
Holistic Interventions:
Diet: lower-carbohydrate diet, with high-quality protein, healthy fats, fiber, probiotic foods
Herbs: ginseng, devil’s club, turmeric, fenugreek, bitter melon, triphala, shilajatu
Nutrients: B complex, vitamin D3, magnesium, chromium, zinc, omega 3 fatty acids
Lifestyle: weight lifting, calisthenics, martial arts, hiking, bicycling, dancing
Osteoporosis Risk
During menopause bones become more fragile and prone to fracture due to the loss of bone density. Reduced estrogen decreases osteoblast activity, which allows for a net increase in bone resorption, leading to a decline in bone density and a higher risk of osteoporosis. In contrast to the usual assumption that this relates to a calcium deficiency, in fact the problem is rooted in the degradation of collagen, which is a general feature of aging, through the gradual accumulation of advanced glycation end-products (AGEs) that damage the protein structure of bone.
Holistic Interventions:
Diet: balanced diet rich in minerals, proteins (e.g. collagen), and high quality fats; phytoestrogenic foods (e.g., legumes, sprouts, flax seed); avoid excess sodium, soft drinks, caffeine, alcohol, antinutrients (e.g. phytates, oxalates, etc.)
Herbs: seaweed (e.g. bull kelp), shatavari, ashwagandha, gokshura, guggulu, licorice, shilajatu, American ginseng, cordyceps, deer antler velvet, shu di huang, he shou wu, milky oats
Nutrients: bone broth, phytoestrogens, vitamin D3, K2, collagen, hydroxy-apatite, magnesium, trace minerals (e.g., boron, strontium), silica
Lifestyle: weight lifting, calisthenics, martial arts, hiking, bicycling
Cardiovascular Disease
The risk of heart disease, high blood pressure, and dyslipidemia increases during perimenopause. Estrogen has various protective effects on the cardiovascular system, particularly on blood vessel function. When estrogen levels drop, several protective mechanisms are lost, resulting in:
Endothelial dysfunction: loss of vasodilation and increased vascular stiffness.
Lipid profile changes: increased LDL, reduced HDL, and elevated triglycerides.
Hypertension: due to increased arterial stiffness, reduced nitric oxide production.
Pro-thrombotic state: increased risk of blood clots.
Insulin resistance: higher risk of type 2 diabetes and metabolic syndrome.
Central obesity: increased visceral fat, indicative of oxidative stress.
Increased sympathetic activity: elevated heart rate and blood pressure.
Holistic Interventions:
Diet: lower-carbohydrate diet, i.e. avoidance of refined carbs and simple sugars; avoidance of grilled meat, lipid peroxides and hydrogenated fats, alcohol, A1 dairy, food additives, pesticides, and herbicides; ensure healthy fats, probiotic foods, dietary fiber; “eat the rainbow”, i.e. red foods (e.g., strawberry, tomato), orange foods (e.g., carrot, squash), green foods (e.g., green beans, broccoli), blue/purple foods (e.g., blueberry, purple cabbage), white foods (e.g., cauliflower, garlic)
Herbs: ginger, cayenne, rosemary, garlic, guggulu, black seed, cinnamon, dan shen, peony, linden, hawthorn, bilberry, ginkgo, amla, arjuna, pomegranate, shilajatu, reishi
Nutrients: B complex, vitamin C, D3, K2, omega 3 fatty acids, magnesium, chromium, selenium, CoQ10, flavonoids
Lifestyle: rest, adequate sleep, nature, spirituality, meditation, muscle-building exercise, breathing exercises (e.g., pranayama), creative release, laughter, community interactions, physical touch
Cognitive Changes
Many women experience cognitive issues during perimenopause, such as difficulty concentrating, forgetfulness, and brain fog. Estrogen supports synaptic function and neurotransmission in the brain, and its decline can lead to cognitive issues like memory loss and brain fog. If hot flashes cause insomnia this can also contribute to cognitive problems from a lack of quality sleep.
Holistic Interventions:
Diet: lower-carbohydrate diet; avoid congesting foods (e.g. flour, cheese, sugar), alcohol, smoking; “eat the rainbow”; useful foods include seaweed, rosehip, jujube, goji, acai, nettle, berries, organ meats, green tea
Herbs: rosemary, bacopa, hawthorn, ashwagandha, calamus, reishi, lion’s mane, cordyceps, rhodiola, psilocybin (microdosing)
Nutrients: B complex, vitamin D3, magnesium, CoQ10, omega 3 fatty acids, phosphatidylserine, L-acetyl carnitine, alpha lipoic acid, grapeseed extract
Lifestyle: regular exercise, quality sleep and rest, nasya (nasal oil application), meditation
Hair and Skin Changes
Thinning hair, dry skin, and increased wrinkles are common due to reduced collagen synthesis and the production of protein-damaging AGEs. Lower estrogen levels reduce the elasticity of collagen and skin, contributing to wrinkles, thinning skin, and hair loss.
Holistic Interventions:
Diet: high quality proteins and fats; mineral-dense foods; avoid sugar, soft drinks, antinutrients (e.g. phytates, oxalates, etc.), alcohol
Herbs: shatavari, dang gui, he shou wu, bhringaraja, peony, vitex, shu di huang, horsetail, nettle, milky oat, American ginseng, seaweed
Nutrients: vitamins A, B (B2, B7, B9, B12), C, D3, omega 3 fatty acids, ceramides, collagen, iron, zinc, selenium, copper, silica, organosulfur compounds (e.g., broccoli sprout powder), trace minerals
Lifestyle: microneedling (dermastamp), bhringaraja taila (herbal oil)
For more information on hair loss, see my comprehensive blog post on holistic solutions for hair loss.
Urinary Issues
Lower estrogen levels can weaken pelvic floor muscles and the urethral lining, leading to increased frequency of urination, urgency, or involuntary leakage due to weakened pelvic support.
Holistic Interventions:
Diet: elimination/challenge diet; protein (collagen), healthy fats
Herbs: shatavari, peony, gokshura, mullein root, nettle root, pipsissewa, cranberry, shilajatu
Nutrients: vitamin D3, magnesium, probiotics, alpha lipoic acid, d-mannose
Lifestyle: Kegel exercises, bladder training, pilates
Feedback please!
If you’re a perimenopausal woman, what kinds of interventions have been most effective for you? What aspects of this transition do you find most surprising or challenging? I’m also curious to hear what you’d like to explore in future posts—on this or any other health subject. Let’s keep the conversation going.












Wow, Todd! I always enjoy your writing, but this is super! As one who has passed thru peri to full menopause, I appreciate your supportive perspective in a personal way. All seasons of life (and all who pass through them) deserve this kind of wholehearted support. Maybe most of all, I appreciate your global view.
I really enjoyed reading this article Todd, a wonderful perspective.
For myself I’m enamoured with Shativari, and avocados and nuts have become a daily treat. I was feeling a lot of tension and heat in my system and these have been a great help so far. I realize this will change as I go further down the perimenopause path but for now they have provided comfort.